The endocrine system works in tandom with the nervous system to help regulate many physiological events. Some notable differences between the two will help understand why both systems may be necessary for regulation of many physiological processes. Events controlled by the endocrine system may appear immediate, they are, in comparison to the nervous system significantly slow. In fact, the endocrine system is designed to carry out physiological events over a long period of time. Some of these events include growth and sexual development among other slow-paced events, unlike the nervous system, whose primary function is to aid in immediate response to both internal and external stimuli, e.g., reflexes and sensory information processing. The endocrine system's means of physiological regulation is hormones, while the nervous system uses electrical impulses (action potentials) and neurotransmitters. Another major difference between the two is how information is transmitted. While the nervous system uses neurons and neurotransmitters to transduce information, the endocrine system is ductless, meaning it is not "wired" like the nervous system. Its hormones are released into the blood stream and searches for cells that bear receptors for that particular hormone. Other notable differences between the two include, as said before, reaction times, location of reactions, and effects on the body's cells. Nonetheless, the two work together to synchronize functions required of the body during times of excitement and sadness, sleep and wake. The remainder of this page will highlight the basics of the endocrine system, i.e., the key structures of the endocrine system, the major hormones involved, their respective places of production, and their effects on cells and organs.
-O. James
© Orin James 2013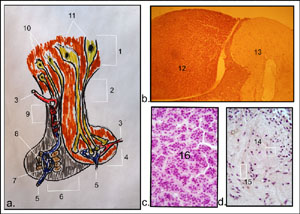 Pituitary Gland and Hypothalamus
Pituitary Gland and Hypothalamus
The collage on the right represents the human pituitary gland connected to the hypothalamus. (a) Drawing of pituitary gland connected to hypothalamus. (b) Photomicrograph of anterior and posterior pituitary lobes, respectively (90x). (c) photomicrograph of anterior pituitary lobe (190x). (d) Photomicrograph of posterior pituitary lobe (190x). To view enlarged image in a new window, simply click on image (photos and drawing by Orin James).
The pituitary gland (hypophysis) and hypothalamus presents us with an example of a direct interaction between the nervous system and the endocrine system. The hypothalamus (1) is referred to as a neuroendocrine gland for both its neural and endocrine function. It forms the root from which the posterior pituitary lobe (4) will grow down. The noticeable down-grown round posterior pituitary lobe remains attached to the hypothalamus via the infundibulum (2), aka connecting stalk. Because the posterior pituitary lobe is ideally a downgrowth of the central nervous system (hypothalamus is part of the base of the brain), it retains the neural connections to the brain, giving the posterior pituitary lobe the epithet neurohypophysis. This neural connection is referred to as the hypothalamic-hypophyseal tract. This tract runs from the neurons of the supraoptic (11) and paraventricular nuclei (12) of the hypothalamus all the way to the posterior pituitary lobe. What is important to note here is that the supraoptic and paraventricular nuclei both synthesize two hormones, antidiuretic hormone (ADH aka vasopressin), and oxytocin, respectively. Once these hormones are synthesized they are then transported along the axons to the posterior pituitary lobe, where they are stored and await a hypothalamic neural stimulus for release (15). The posterior pituitary lobe does not have hormone producing cells.
The anterior pituitary gland, also referred to as the adenohypophysis (6), stems from the oral mucosa and during development attaches itself to the posterior lobe (neurohypophysis). Prolonged attachment leads to the anterior lobe losing its connection to the oral mucosa and adhering to the neurohypophysis. Therefore, the anterior lobe has no direct neural connection to the brain like the neurohypophysis, rather it has a vascular connection. This vascular connection is referred to as the hypophyseal portal system (9). It is comprised primarily of capillary beds that feed into veins and arteries. Control hormones, produced in the hypothalamus, which will either have an inhibitory or releasing effect, will be released from the hypothalmus and enter this hypophyseal portal system. After these hormones circulate the hypophyseal portal system they will enter the adenohypophysis (anterior pituitary lobe) and have its effects on the hormones produced by the adenohypophysis. The adenohypophysis is responsible for producing six hormones, which I will discuss shortly, but first a look at the collage on the right:
-O. James
© Orin James 2013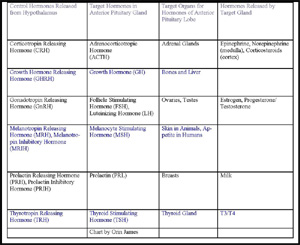 Control Hormones of the Hypothalamus
Control Hormones of the Hypothalamus
Chart on the right details the control hormones of the hypothalamus and their target hormones in the anterior pituitary lobe, along with the anterior pituitary lobe's target organ. To view enlarged image in a new window, simply click on image (chart constructed by Orin James).
As mentioned in the discussion on the adenohypophysis and the hypothalamus, the ventral region of the hypothalamus is responsible for synthesizing control hormones that will be channeled via the hypophyseal portal system to the adenohypophysis (anterior pituitary lobe), where they will lead to the release or inhibition of hormones produced in the adenohypophysis. These control hormones include:
-O. James
© Orin James 2013The above sections have provided you with brief descriptions of the six hormones produced in the anterior pituitary gland. Here I will provide further discussion of each. As you read this section, you will find that some of these hormones only function to lead to the release of other hormones from target organs. This role makes those hormones tropic hormones. Four of the six hormones discussed are tropic hormones (thyroid stimulating hormone, adrenocorticotropic hormone, follicle stimulating hormone and luteinizing hormone.
Adrenocorticotropic hormone is released from the adenohypophysis upon interaction with corticotropin releasing hormone (CRH), which is released from the ventral region of the hypothalamus (see discussion on control hormones of the hypothalamus above). High blood levels of ACTH will lead to a negative feedback loop, which in turn will block further release of CRH.
Growth hormone release or inhibition is controlled by two ventral hypothalamic hormones, namely GH-RH and GH-IH (see discussion on control hormones of the hypothalamus above).
-O. James
© Orin James 2013The posterior pituitary lobe or neurohypophysis is, again, responsible for storing the hormones produced in the supraoptic and paraventricular nuclei of the hypothalamus. THE POSTERIOR PITUITARY LOBE DOES NOT PRODUCE HORMONES! The two hormones that are stored in the neurohypophysis are antidiuretic hormone (ADH) and oxytocin. Let's look at the roles of each.
-O. James
© Orin James 2013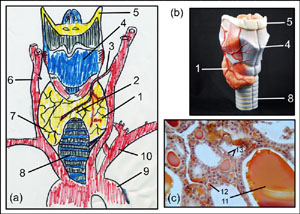 The Thyroid Gland, Thyroid Hormone and Calcitonin
The Thyroid Gland, Thyroid Hormone and Calcitonin
The collage on the right represents the human thyroid gland attached to the trachea. (a) Drawing of thyroid gland attached to the trachea with surrounding blood vessels. (b) Photo of model containing thyroid gland attached to trachea. (c) photomicrograph of thyroid gland (190x). To view enlarged image in a new window, simply click on image (photos and drawing by Orin James).
The thyroid gland is considered the largest endocrine gland in the body. It is a bi-lobed gland (1) located on the trachea slightly below the larynx. The two lobes are connected at what is called the isthmus (2). Both lobes are composed primarily of follicle cells, which produce thyroglobulin (11). The lumen of these follicles store colloid, which consists of thyroglobulin molecules with iodine attached. The idoine bound to thyroglobulin makes up the Thyroid Hormones (TH). More on TH below. The parafollicular cells (12) are responsible for producing calcitonin.
Thyroid hormones (TH) are the body's primary metabolic hormones. These include two iodine-containing amine hormones, thyroxine (T4) and triiodothyronine (T3). The thyroid follicles will secrete mostly the T4 hormone, while T3 is formed at the target tissues, as it converts from T4 to T3. These hormones function in a similar fashion to steriod hormones, i.e., they bind to an intracellular receptor, activates genes, which in turn will lead to transcription and translation of these genes into a protein. As stated, these hormones are affect every cell in the body. Therefore, these hormones will be responsible for promoting normal: heart function, muscular development, bone growth and maturation, gastrointestinal motility, and tone, secretion of digestive juices, skin hydration, glucose catabolism, body temperature and development of nervous system, just to name a few.
Calcitonin is the other hormone produced by the thyroid gland. Its primary function is to lower blood calcium levels. It antagonizes parathyroid hormone (PTH). It does this by inhibiting osteoclast activity, bone resorption and release of calcium from the bone matrix.
IllnessesSome notable illnesses associated with the thyroid gland include myxedema, goiter, cretinism and Graves' disease. myxedema literally means mucous swelling. Some of the symptoms include mental sluggishness, low metabolic rate, chill, dry skin, puffy eyes, and constipation. This may occur if the thyroid is defective in some way or if there is inadequate release TRH orTSH. If there is a lack of iodine in the thyroid follicles and the anterior pituitary lobe continues to release TSH, the thyroid gland's follicles will accumulate excessive unusable colloid, which will lead to swelling. This noticeable protrusion of the thyroid gland through the neck may indicate the condition called goiter. Cretinism is found in infants. In its most severe form the infant may be mentally retarded and have a short disproportionately sized body. Its tongue and neck may also appear thick. The three aforementioned illnesses all fall under the larger group of hypothyroid disorders. The one that falls in the division of hyperthyroid disorders is Graves' Disease. This is an autoimmune disorder, in which abnormal antibodies are produced and are directed against the follicle cells. However, instead of attacking the follicle cells, these antibodies "act" like TSH and stimulate TH release, thereby increasing metabolic rate, sweating, and nervousness. An obvious symptom of this is protrusion of the eyes.
Collage on right:
-O. James
© Orin James 2013These glands are pyramid shaped and reside atop the kidneys, hence they are also called the suprarenal glands. Each of these glands can be viewed as being two endocrine glands due to its internal make up. One adrenal gland contains an inner region called the adrenal medulla, which is comprised primarily with nervous tissue, making this region a functional part of the sympathetic nervous system. The outer region, adrenal cortex forms the bulk of the gland and is comprised of glandular tissue. Both regions produces its own set of hormones.
The adrenal medulla stores cells called medullary chromafin cells. These cells surround blood rich capillaries and sinusoids. They are essentially modified postganglionic sympathetic neurons that produce the catecholamines epinephrine and norepinephrine (NE) via tyrosine and dopamine to NE to epinephrine, respectively. Both epinephrine and norepinephrine are released during a fight or flight response, however, epinephrine is a stronger stimulator of bronchial dilation, metabolic activities and increased blood flow to skeletal muscles and the heart. Norepinephrine plays a more important role in peripheral vasoconstriction and blood pressure. In the clinical setting, epinephrine is used to stimulate the heart and dilate bronchioles during an acute asthma attack.
The adrenal cortex produce steroid hormones called corticosteroids. There are three regions of the adrenal cortex. Each of these regions is responsible for producing a specific type of hormone. The zona glomerulosa is responsible for producing mineralcorticoids, which help control the balance of minerals and water in the blood. The zona fasciculata is responsible for producing glucocorticoids, which function as metabolic hormones. The zona reticularis is responsible for producing gonadocorticoids, which function as sex hormones.
Mineralcorticoids are needed to regulate electrolyte concentrations in extracellular fluids. The most abundant cation in extracellular fluid is Na+. Where Na+ goes, water follows. Therefore, it is not surprising that Na+ in turn determines the volume of extracellular fluid. Changes in Na+ levels can alter blood pressure and blood volume. Another crucial cation is K+. The extracellular concentration of K+ determines how easily an action potential is generated. Therefore, regulation of these two ions is critical. The hormone that regulates these two ions is aldosterone. Aldosterone reduces excretion of Na+ from the body by stimulating reabsorption of Na+ and water retention, while eliminating K+ at the renal tubules. Aldosterone also aids in Na+ reabsorption from saliva, sweat and gastric juice. More on aldosterone is discussed with the renin-angiotensin-aldosterone mechanism in the physiological mechanisms of hormones on cells below.
Glucocorticoids directly influence metabolism of most body cells and aid in resisting stress. The glucocorticoid hormones include cortisol, cortisone and corticosterone. Of the three glucocorticoids, cortisol is the most important in humans, as it is the only one secreted in significant amounts. they are all steroid hormones and therefore, activate genes in target cells. Under stressful conditions, cortisol will be released, which in turn will lead to gluconeogenesis, the generation of glucose from proteins and fats. Cortisol will influence stored proteins to break down for repair or to make enzymes for metabolic processes. Cortisol will also mobilize fatty acids from adipose tissue and encourage their use for energy. Cortisol also strengthens the sympathetic nervous system's vasoconstrictive effects. Cortisol also raises blood pressure and circulatory efficiency to ascertain nutrients reach cells.
Gonadocorticoids released by the adrenal cortex are weak male sex hormones known as androgens. These include androstenedione and dehydroepiandrosterone (DHEA). Most of these hormones are converted to the stronger male hormone testosterone in tissue cells. When compared to the amount of gonadocorticoids produced in the gonads during late puberty and adulthood, the amount produced by the adrenal cortex is insignificant. It is still unclear, however, what the exact role of the gonadocorticoids is. It is clear, nonetheless, that they contribute to axillary and pubic hair development. In adult women they are thought to contribute to the sex drive and account for estrogens produced post-menopause.
The pancreas differs from the other glands discussed above in that it serves not only an endocrine function, but also an exocrine function, that is , it has ducts serving as conduits for the passage of substances. In the case of the pancreas, its exocrine function serves the digestive system. The pancreas is comprised primarily of acinar cells, which produce the enzyme-rich juice used for digestion and is passed into the small intestines via ducts. Other cell types that comprise the pancreas include the alpha and beta cells. Both of these cell types reside in pancreatic islets (islets of Langerhans), which surround the acinar cells. The alpha cells produce the hormone glucagon, while the beta cells produce the hormone insulin. These hormones antagonize each other to balance blood glucose levels.
Glucagon is used to breakdown glycogen into glucose (glycogenolysis), synthesize glucose from lactic acid and from noncarbohydrate molecules (gluconeogenesis), and release glucose into the blood via liver cells, all leading to blood glucose levels to rise. Glucagon may be released due to humoral stimuli. If blood glucose levels are low, or levels of amino acid rise, alpha cells may release glucagon. However, the sympathetic division of the autonomic nervous system may also lead to the release of glucagon.
Insulin is first produced as part of a larger polypeptide chain known as proinsulin. Just before insulin is released from the beta cells, it is cut from proinsulin and made active. Insulin's effects are readily seen after one eats a meal rich in carbohydrates. Insulin is responsible for enhancing cell membrane permeability for allowing glucose into the cell. Insulin also blocks the breakdown of glycogen into glucose. It also blocks the conversion of amino acids or fats to glucose. If blood glucose levels remain high, this may be indicative of diabetes mellitus. If one lacks insulin, this condition is referred to as diabetes type I. If one, however, has insulin available, and it appears deficient, this may be indicative of diabetes type II.
Physiological Mechanisms of Hormones on Cells |
-O. James
© Orin James 2013