Urinary System Basics
|
Introduction
The urinary system is responsible for removing toxins, metabolic wastes and excess ions from the blood stream by
way of urine. The primary organs producing urine are the kidneys. About 200 liters of fluid is filtered by the kidneys on a daily basis.
These two bean shaped organs are positioned posterior to the peritoneal cavity, anterior to the dorsal wall and at about the height of the
12th ribs and spans between the T12 and L3 vertebrae. In summary the kidneys regulate the total volume of water in the body and the total
concentration of solutes in that water (osmolality). They regulate the various ion concentrations in the
extracellular fluids. They help maintain long-term acid-base balance. They remove foreign substances such as drugs
and toxins. They produce renin and erythropoietin, which regulate blood pressure and red blood production, respectively.
They help produce sugars via gluconeogenesis and convert vitamin D into its active form. While the kidneys
form the urine, they are not, however, responsible for removing the urine from the body. The urinary system
has three other important components namely: ureters, which are responsible for draining the urine from
the kidneys into the urinary bladder, which temporarily stores the urine produced in the kidneys. Lastly,
the urine is drained from the urinary bladder and voided from the body by way of the urethra, the last major
component of the urinary system.
The remainder of this page will highlight the structural features of the components of the urinary system and some of their
functional roles.
-O. James
© Orin James 2013
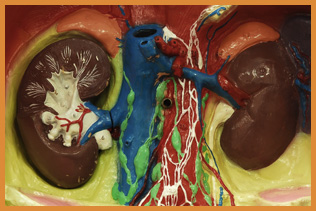
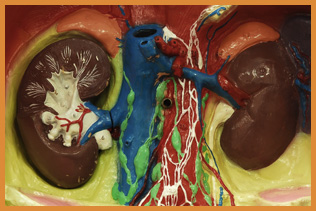
 Gross Anatomy of Kidney
Gross Anatomy of Kidney
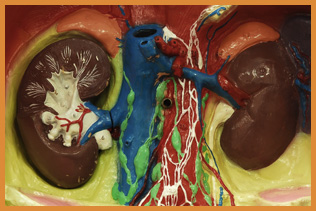
The collage on the right contains a frontal section of a sheep's kidney (A) and a detailed frontal section
of a right kidney (B).
Click on image for larger representation. Photo by Orin James.
As mentioned in the introduction, the kidneys are bean shaped organs used to filter the body's blood supply.
It is positioned posterior to
the peritoneal cavity, anterior to the dorsal wall and at about the height of the 12th ribs and spans
between the T12 and L3 vertebrae. A frontal section of the kidneys will reveal the following important
components:
- Renal Cortex:
This is the most light colored and superficial region of the kidney and contains a major portion
or the nephron and all cortical radiate arteries (2).
- Cortical Radiate Arteries:
These arteries supply the renal cortex with oxygen rich blood, received from the arcuate arteries (4),
which receives oxygen rich blood from the interlobar arteries (7), which will receive oxygen rich blood
from the several segmental arteries (8), which receives oxygen rich blood from the renal artery (9). The
renal artery will get its oxygen rich blood supply from the aorta.
- Cortical Radiate Veins:
These veins drain blood from the renal cortex (1) into the arcuate veins (5) then the interlobar
veins (6), before it exits via the renal vein (10).
- Arcuate Arteries:
These arteries feed oxygen rich blood to the cortical radiate arteries (2) and receive oxygen rich blood from the interlobar arteries (7), which will receive oxygen rich blood
from the several segmental arteries (8), which receives oxygen rich blood from the renal artery (9). The
renal artery will get its oxygen rich blood supply from the aorta.
-
Arcuate Veins:
These veins receive oxygen poor blood from the renal cortical veins (3) and drain it into the interlobar
veins (6), before it exits via the renal vein (10).
-
Interlobar Veins:
These veins receive oxygen poor blood from the arcuate veins (5) and drain it into the
renal veins.
-
Interlobar Arteries:
These arteries will receive oxygen rich blood from segmental arteries (8) and
feed it into the arcuate arteries (4).
- Segmental Arteries:
These arteries will recieve oxygen rich blood from the renal
arteries (9) and feed it into the interlobar arteries (7)
- Renal Arteries:
These arteries will recieve oxygen rich blood from the aorta and
feed it into the segmental arteries (8), which will feed it into the interlobar arteries (7),
which will feed it into the arcuate arteries (4), which will feed it lastly into the cortical
radiate arteries (2).
- Renal Vein:
This vein removes oxygen poor blood from the kidneys. It receives this
blood from the interlobar veins (6), which receive oxygen poor blood from the arcuate veins (5), which
receive oxygen poor blood from the cortical radiate veins (3).
- Renal Pelvis:
This structure functions as a funnel to drain
the urine produced into the ureters (12)
- Ureter:
This structure is responsible for transporting urine from
the kidney into the bladder.
- Minor Calyx:
This structure is a branch of the renal pelvis (11). It collects
urine from the renal pyramids (14) and drain it into the renal pelvis (11).
- Renal Pyramids:
The renal pyramids are located in the medullary region of
the kidney (16). They appear striated because they contain the loops of the nephron.
Each pyramid has a base, which points towards the renal cortex (1) and an apex
that points into the minor or major calyces (13, 17).
- Renal Column:
These structures separate the renal pyramids (14).
- Renal Medulla:
This region is deep to the renal cortex (1) and appears darker/redder
than the renal cortex (1). It is comprised of the renal pyramids (14).
- Major Calyx:
This structure is a branch of the renal pelvis (11). It collects
urine from the renal pyramids (14) and drain it into the renal pelvis (11).
-O. James
© Orin James 2013
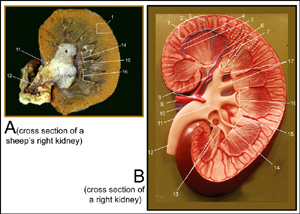
 General Structure of the Nephron
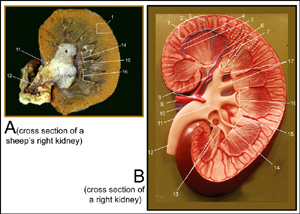
General Structure of the Nephron
The image on the right is that of a nephron. To view enlarged image in a new window, simply click on image. (image by Orin James).
Millions of nephrons can be found in the kidney. These are the functional units of the kidneys that produce urine. Majority of the components that comprise
the nephron can be found in the renal cortex. These include the renal corpuscle, proximal and distal convoluted tubules and parts of the nephron loop and
collecting duct. The nephron loop and collecting duct continue into the renal medulla. It is important to note that although the major components of the nephron
are found in the cortex, some nephrons may have these closer to the cortex-medulla junction than to the cortex. In the case where the major components are closer
to the cortex-medulla junction, these will be called juxtamedullary nephrons. These tend to have a longer nephron loop/Loop of Henle and its efferent artery will
feed into the vasa recta. In the case where the major components of the nephron may be found further from the cortex-medulla junction, these will be called
cortical nephrons. They tend to have a shorter nephron loop/Loop of Henle than the juxtamedullary nephron. Their efferent arteries feed into peritubular
capillaries rather than the vasa recta capillaries. See The Renal Corpuscle here.
- Renal Cortex:
See Gross Anatomy of Kidney
- Cortical Radiate Veins:
See Gross Anatomy of Kidney
- Renal Corpuscle:
This structure is responsible for starting the blood filtering process. It
is comprised of the Glomerulus (a capillary bed comprised of fenestrated capillaries) and the Bowmans/Glomerular
Capsule, which surrounds the glomerulus. Both strucures are discussed in detail here: The Renal Corpuscle
- Cortical Radiate Arteries:
See Gross Anatomy of Kidney
- Renal Corpuscle:
See 3. This structure is responsible for starting the blood filtering process. It
is comprised of the Glomerulus (a capillary bed comprised of fenestrated capillaries) and the Bowmans/Glomerular
Capsule, which surrounds the glomerulus. Both strucures are discussed in detail here: The Renal Corpuscle
- Proximal Convoluted Tubule:.
This is beginning of the Renal Tubule. It is responsible for
reabsorption of sodium ions primarily via active transport, reabsorption of glucose, amino acids, vitamins and some
ions via secondary active transport using sodium ions, reabsorption of chloride, potassium, magnesium, calcium and other ions
via passive diffusion, reabsorption of bicarbonate via secondary active linked to hydrogen secretion and sodium reabsorption,
reabsorption of water via osmosis, reabsorption of lipid-soluble solutes via passive diffusion driven by concentration gradient,
and reabsorption of urea via passive diffusion driven by chemical gradient.
- Loop of Henle/Nephron Loop (Descending Limb):
This is the next region of the Renal Tubule. It is comprised
of two limbs, the descending and ascending limbs. The descending limb is primarily responsible for the reabsorption of water via osmosis.
Calcium and magnesium will diffuse passively based on electrochemical gradient. More
on the importance of the Loop of Henle in the Physiology of Renal System below.
- Loop of Henle/Nephron Loop (Ascending Limb):
This is the next region of the Renal Tubule. It is comprised
of two limbs, the descending and ascending limbs. The ascending limb is primarily responsible for the reabsorption of sodium, chloride and potassium
via secondary active transport using the sodium-potassium pump. Calcium and magnesium will diffuse passively based on electrochemical gradient. More
on the importance of the Loop of Henle in the Physiology of Renal System below.
- Distal Convoluted Tubule:
This is the last region of the Renal Tubule. Reabsorption of sodium and chloride
occurs here via active sodium transport at basolateral membrane and secondary active transport at apical membrane via the sodium-chloride
symporter and channels, which may be aldosterone-regulated at the distal end. Reabsorption of calcium may be done passively via PTH-modulated
channels in the apical membrane. In the basolateral membrane calcium may be reabsorbed via the primary and secondary active transport
mechanism (antiport with sodium).
- Collecting Duct:
The collecting duct does as its name implies. It collects the filtrate and bring it to the medullary pyramids,
where they will fuse into the calyx and drain the urine into the renal pelvis. Reabsorption of sodium, potassium, bicarbonate, chloride, water and urea occurs here.
Sodium is transported actively and requires the presence of aldosterone while potassium is both reabsorbed and secreted and dependant on aldosterone as well.
Chloride and bicarbonate passively diffuse. Reabsorption
of water is done via osmosis and facultative reabsorption. ADH is required to insert aquaporins onto the collecting duct for reabsorption of water. Lastly,
urea is reabsorbed via facilitated difussion in response to the concentration gradient in the deep medulla region.
- Arcuate Artery:
See Gross Anatomy of Kidney
- Arcuate Vein:
See Gross Anatomy of Kidney
- Renal Medulla:
See Gross Anatomy of Kidney
-O. James
© Orin James 2013
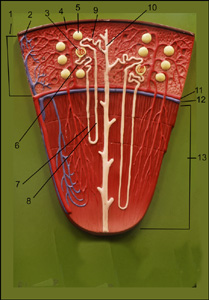
 The Renal Corpuscle
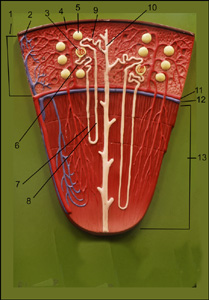
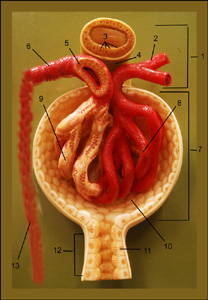
The Renal Corpuscle
The image on the right is the juxtaglomerular complex and the renal corpuscle. To view enlarged image in a new window,
simply click on image. (image by Orin James).
As stated previously, the renal corpuscle is the site where filtration of blood will begin. Aiding this process is the
juxtaglomerular complex. More on these structures below.
- Juxtaglomerular Complex:
This structure provides blood to the renal corpuscle via of the afferent vessels. It also has
the efferent vessels, which will bring blood to the peritubular capillaries (cortical nephrons) or vasa recta capillaries (juxtamedullary nephrons).
The juxtamedullary complex also has several cell types important for detecting systemic blood pressure and ion content in the blood.
- Afferent Arterioles:
These arterioles collect blood that needs to be filtered from the cortical radiate arteries.
See Gross Anatomy of Kidney.
- Macula Densa Cells:
These are chemoreceptor cell types that are closely packed in the ascending limb of the nephron loop/Loop of Henle.
They are responsible for detecting the NaCl content of the filtrate entering the distal convoluted tubule.
- Extraglomerular Mesangial Cells:
These cells reside between the arterioles (6 & 2) and the macula densa cells (3). We are
still looking at the ascending limb. These cells may be working to provide regulatory signals between the macula densa and granular cells.
- Granular Cells: These cell types are found in the arteriole walls. They have
secretory granules containing the enzyme renin. These cells act as mechanoreceptors that
detect blood pressure in the afferent arteriole wall.
- Efferent Arteriole:
This arteriole will feed blood that is being filtered in the glomerulus, into the peritubular capillary beds (cortical nephron) or vasa recta
capillary beds (juxtamedullary nephrons), where reabsorption of important substances for blood will be reabsorbed.
- Glomerular/Bowman's Capsule:
This structure along with the glomerulus (8) comprise the renal corpuscle.
There are two layers to this capsule. The first one not obvious is the parietal layer, which forms the structure of the capsule.
This is made clear as we notice the capsular space (10) between the glomerulus (8) and the capsule (7). The other layer of the
capsule is the visceral layer, which directly interacts with the glomerulus. This layer is comprised of
podocytes (9). These cells have filtrate slits, which allow filtrate to enter the capsular space (10).
- Glomerulus:
This is the capillary bed of the renal corpuscle. It is comprised of fenestrated capillaries,
which provides pores, through which allows protein-free fluids/filtrage to pass from the blood into the capsular space (10). The filtering of blood at this point
is known as glomerular filtration.
- Podocyte:
These cell types are found on the visceral layer of the Bowman's Capsule (7) and provide slits for
protein-free fluid to pass into the capsular space (10).
- Capsular Space:
This space is where protein-free fluids/filtrate will enter.
- Proximal Tubule Cell:
These cells line the proximal convoluted tubule. See General Structure of Nephron here.
- Proximal Tubule:
This tube will collect substances from the blood that was filtered by the glomerulus, a process known as glomerular filtration. These substances may be reabsorbed by the peritubular capillary
(cortical nephrons) or vasa recta (juxtamedullary nephrons), a process known as tubular reabsorption. Substances may also be selectively added to the tubule via secretion from
the peritubular/vasa recta capillaries. This process is known as tubular secretion. The substances that are not reabsorbed by the peritubular/vasa recta capillary beds will be used
to form urine.
- Peritubular/Vasa Recta Capillary Beds:
Regardless of the nephron type (cortical or juxtamedullary), this capillary bed will receive blood that is deprived ionic substances. This capillary
bed resides close to the tubule, where it may reabsorb some of those substances or secrete unwanted substances into the tubule. This capillary bed will then feed that blood into the cortical radiate vein to
return to the rest of the body.
-O. James
© Orin James 2013
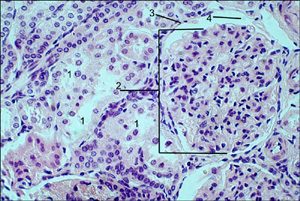 Microscopic Anatomy of Kidney (Renal Corpuscle)
Microscopic Anatomy of Kidney (Renal Corpuscle)
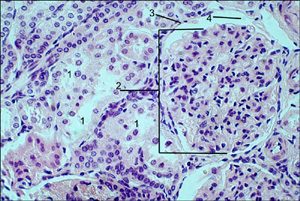
The image on the right is a photomicrograph of the tissue found in the renal cortex of the kidney (200x). It shows the renal corpuscle, proximal and distal convoluted tubles of the nephron.
To view enlarged image in a new window, simply click on image. (image by Orin James).
- Distal Convoluted Tubules
- Glomerulus
- Parietal Layer of Glomerular/Bowman's Capsule:
- Glomerular/Bowman's Capsule Space
-O. James
© Orin James 2013
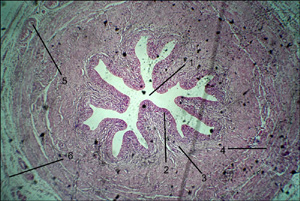 Microscopic Anatomy of Ureters
Microscopic Anatomy of Ureters
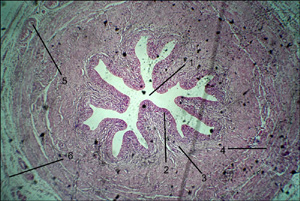
The image on the right shows a photomicrograph of a cross section of the ureter.
To view enlarged image in a new window, simply click on image. (image by Orin James).
The ureters are responsible for conveying urine from the kidneys to the bladder. The
bladder has three layers of tissue: Mucosa, which is composed of a transitional epithelium
and lamina propia. The second layer is Muscularis, which is composed of internal longitudal
and external circular smooth muscle layers. This layer allows urine to be actively transported to
the bladder via muscular contractions. The third layer is Adventitia, which is the outermost
covering of the ureter.
- Lumen
- Transitional Epithelium of Mucosa Layer
- Lamina Propria of Mucosa Layer
- Longitudinal Layer of Muscularis
- Circular Layer of Muscularis
- Adventitia
-O. James
© Orin James 2013
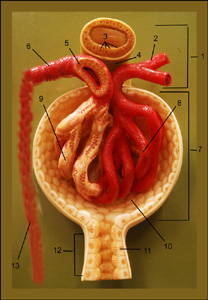
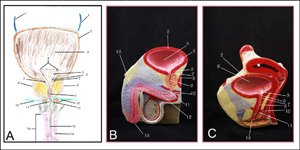 Ureters/Bladder/Urethra
Ureters/Bladder/Urethra
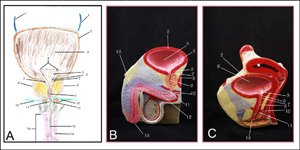
The image on the right shows various representations of the ureters, bladders and urethra in the male (A, B) and female (C).
To view enlarged image in a new window, simply click on image. (image by Orin James).
Urine produced in kidneys are then drained, of ureters (1), into the bladder, which is a smooth, collapsible, muscular sac that temporarily stores urine ( 2, 3, 4,5, & 6).
The bladder can collect up to about 200ml, before stretch receptors are activated. At this point impulses caused by contractions are sent
to the parasympathetic division of the nervous system. As contractions continue urine may be forced past the internal sphincter (7)
into superior part of the urethra. At this point the individual may feel the need to void. The individual may, however, not find it
convenient to void at that point and inhibit the opening of this sphincter. If voiding is inhibited, bladder contractions may cease temporarily and the bladder may store another 200 to 300 ml of urine. After this
amount has been collected, the micturition reflex will be once again initiated. Once voiding has been initiated, urine will leave the body via the
urethra. The length of the urethra differs between males and females. In males the urethra also runs the length of the penis and may reach a length of
about 8 inches, while in females the urethra lies anterior to the vaginal opening and posterior to the clitoris, extending only about 1.5 inches long.
- Ureters:
These are conduits for urine being drained from the kidneys into the bladder (one ureter per kidney).
- Detrusor Muscle:
This is one of three muscular layers of the bladder. The other two layers include a thick mucosa and a fibrous adventitia at the
surface.
- Rugae:
These are folds into which the bladder will collapse when empty. When empty the bladder will collapse into a pyramidal shape.
- Ureteric Orifices:
Openings for the ureters to drain urine.
- Trigone:
This triangular region has openings for the ureters and urethra.
- Neck of Bladder:
This region allows urine to flow from the bladder into the urethra.
- Internal Urethral Sphincter:
This sphincter is involuntary and is controlled by the autonomic nervous system. It prevents leaking of
urine from the bladder before voiding, when closed.
- Prostate:
More on this on Reproduction Page
- Prostatic Urethra:
This region of the urethra is about 2.5 cm long and runs within the prostate (males only).
- Urogenital Diaphragm
- External Urethra Sphincter and Intermediate Part of Urethra:
This sphincter is voluntarily controlled and can be opened when an individual would
like to voluntarily void. The intermediate part of the urethra runs through the urogenital diaphragm and extends about 2 cm from the prostate to the
beginning of the penis (males only).
- Spongy Urethra:
This region of the urethra continues from the intermediate part of the urethra and opens at the tip of the penis via the
external urethral orifice (15).
- Erectile Tissue of Penis:
More on this on Reproduction Page.
- Penis:
More on this on Reproduction Page.
- External Urethral Orifice:
This is the exit point of urine from to body to the external environment.
-O. James
© Orin James 2013
Urine Basics
By performing a urinalysis, one can easily study the contents of their own urine,
the voided product of kidney
filtration. Some of the characteristics
and substances tested for include pH
(usually between 4.5 and 8, average about 6), color (usually clear to pale
yellow to amber),
specific gravity (usually between 1.001 and 1.030)
inorganic substances such as sulfates, phosphates,
chlorides, and nitrites.
One can also test for organic components like urea, glucose, albumin, ketone bodies,
bilirubin, leukocytes
bilirubin and urobilinogen. If you are
wondering what type information we can gain from such
a test, here is a run down:
- Glycosuria:
Excess glucose in the blood.
Highly indicative of
diabetes mellitus.
- Albuminuria:
Presence of Albumin in urine indicates problems may exist with the glomerulus
(not filtering macromolecules), or bacteria. However, Albumin in urine may be present in healthy pregnant women.
- Ketonuria:
Presence of acetoacetic acid, beta-hydroxbutyric acid or acetone in urine
indicates abnormal metabolism of fats,
which may be due to starvation or a low carbohydrate diet.
- Hematuria:
Presence of red blood cells in the blood may indicate a
pathology in the urinary
tract or menstruation in healthy females.
- Hemoglobinuria:
Presence of hemoglobin or
fragments thereof may be due to snake bites,
transfusion, burns or renal diseases.
- Nitrites:
Presence of nitrites indicate a bacterial infection, usually E. coli or other
germ-negative rods.
Nitrites usually reflect a bladder infection.
- Bilirubinuria:
Presence of bile pigments usually a liver pathology
(hepititis, cirrhosis, bile duct blockage)
- White Blood Cells:
Presence of white blood cells indicates an inflammation of the urinary tract.
High levels often reflect hepititis A or cirrhosis.
There you have it! By simply studying the voided content of the kidney,
we can gain insight into whether or other structures of the body are
functioning properly.
Be sure to have your urine tested during a regular check up!☻
Physiological Mechanisms of Urinary System
|
Coming soon...
-O. James
© Orin James 2013
 Gross Anatomy of Kidney
Gross Anatomy of Kidney
 General Structure of the Nephron
General Structure of the Nephron
 The Renal Corpuscle
The Renal Corpuscle
 Microscopic Anatomy of Kidney (Renal Corpuscle)
Microscopic Anatomy of Kidney (Renal Corpuscle)
 Microscopic Anatomy of Ureters
Microscopic Anatomy of Ureters
 Ureters/Bladder/Urethra
Ureters/Bladder/Urethra